
Senator Bill Cassidy (R-LA) discussing the need to end surprise billing in a hearing. Senator Cassidy, an M.D., is one of the leaders who got the serious, bipartisan discussion of ending surprise billing going in Congress.
On December 11th we got advanced notice that the leaders of the four key committees in Congress have reached a bipartisan agreement to end surprise billing. Here are the key provisions of the new surprise billing legislation proposed by the Republican and Democratic leaders of those congressional committees.
Ends Surprise Billing for Patients
Most importantly, like all five bipartisan bills we reviewed in our brief, the new legislation would end surprise bills for patients. Going forward, patients would only be responsible for paying their usual in-network cost-sharing amount (e.g. co-pays and deductibles).
Most Comprehensive in Types of Surprise Bills in Stops
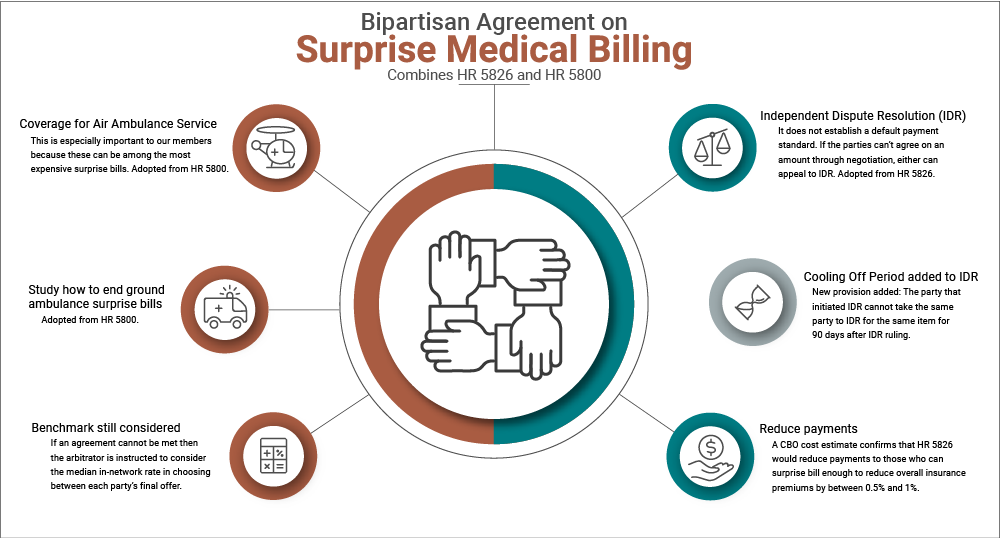
The agreement is a compromise between the House Education & Labor Committee’s bill (H.R. 5800) and the House Ways & Means Committee’s bill (H.R. 5826). At 81%, HR 5800 received the broadest support from our members of any of the five bills we reviewed in our brief. Because members were most concerned with ending surprise billing for patients, one of the most important reasons for members’ support for HR 5800 was that it was the most comprehensive in the types of surprise bills it would end. The new agreement adopts the two key provisions on this point that were in H.R. 5800 and that were missing from H.R. 5826. First, the new legislation takes from HR 5800 the provision to end surprise billing from air ambulance services. This is especially important to our members because these can be among the most expensive surprise bills. Ninety-four percent of our you supported ending surprise bills for air ambulances. H.R. 5826 would have only studied ways to end air ambulance surprise bills. Second, the new agreement adopts H.R. 5800’s provision to study how to end ground ambulance surprise bills (H.R. 5826 left ground ambulances completely unaddressed).
New Provision to Make Sure an IDR-Only Approach Keeps Premiums Down for Patients
H.R. 5826 received much less support from our members (35%) than H.R. 5800 (81%) largely because it was less comprehensive in the types of surprise bills it would have ended, which has been addressed in the new agreement. Another reason many of you supported H.R. 5800 over H.R. 5826 is that you preferred the mechanism by which the amount an insurer should pay an out-of-network provider is determined. H.R. 5800 combined payment standards with Independent Dispute Resolution (IDR). It established the median in-network rate for a given service in a given geographic area as the payment standard that could then be appealed to arbitration if either party disagreed with that outcome for particular cases. The new agreement follows H.R. 5826’s IDR-only approach. It does not establish a default payment standard. If the parties can’t agree on an amount through negotiation, either can appeal to IDR.
The new agreement, however, substantially improves on the IDR-only approach in the eyes of many. The important new provision is that the party that initiated IDR cannot take the same party to IDR for the same item for 90 days after an IDR ruling. Since the arbitrator is instructed to consider the median in-network rate in choosing between each party’s final offer, the negotiations “in the shadow of IDR” should increasingly reflect the median in-network rates over time that H.R. 5800 established as a payment standard. That should help keep IDR from inflating costs for insurers that would be passed along to patients in the form of higher premiums.
Conclusion
While some of the specific provisions in the new agreement announced on Friday do not align precisely with where most CommonSense American members came out, it does reflect a broad theme in our members’ open-ended responses. Many of you advised Congress not to let perfection on the details be the enemy of passing a good bill immediately. As many of you reasonably argued, the status quo of allowing out-of-network providers to treat patients without their knowledge or consent and then charge whatever they wanted is outrageous. There are several approaches that would be much preferable to letting this continue. By immediately passing this new proposed legislation, Congress would end the egregious practice of surprise billing for patients and would provide a serviceable means of resolving how much insurers pay out-of-network medical providers.

